Introduction
Leprosy has a rich history dating to biblical times.
“Leper†is an ancient term used to identify patients with leprosy who were severely stigmatized by the deformity that resulted from Mycobacterium leprae infection.
In the clinical context, the term Hansen’s disease should be used instead of leprosy. Gerhard Henrick Armauer Hansen, a Norwegian physician, discovered the microbe in 1874 just before Koch’s discovery of Mycobacterium tuberculosis.
Epidemiology
In Mexico, in the last 16 years the prevalence of Hansen’s disease has been reduced about 95%, from 16,694 reported cases in 1990 to 820 reported cases in 2006. The World Health Organization (WHO) established the goal of eliminating leprosy as a public health problem by the year 2000, with “elimination” defined as a reduction in prevalence to <1 case per 10,000 population in all endemic countries. The six countries with the highest rates of endemic leprosy in 2001 are: Brazil, India, Madagascar, Mozambique, Myanmar, and Nepal
Transmision
This disease is probably spread by the respiratory route, like tuberculosis.
Risk Factors
Close contact
Older persons
Impaired cell mediated immunity
Clinical manifestations
The cardinal manifestations of leprosy are infiltrative skin lesions, hypoesthesia, and peripheral neuropathy
The clinical manifestations of leprosy are closely related to the polarity of the cellular immune response to M. leprae in the patient.
The history of a patient with suspected leprosy should include whether the person has resided in an area with high prevalence and whether the person has been previously diagnosed or treated for leprosy. Certain patients may deny knowledge of a prior diagnosis or may report that skin lesions or neuropathy or both are acute, as they wish to avoid the stigma of a diagnosis of leprosy, even in emigrants to developed countries.
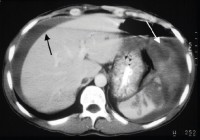
If lepromatous leprosy is left untreated, it can progress to “leonine†facies as seen in the following images.


Diagnosis
This includes physical exam and skin biopsy.
Treatment
Once monthly: Rifampin, Dapzone and Clofazimine for two years and then stop.
Daily: Sulfone and Clofazimine for two years and then stop.