Gallstone Ileus is an infrequent cause of mechanical bowel obstruction. It is caused by an impaction of a gallstone in the terminal ileum by passing through a billiary-enteric fistula (often from duodenum). It occurs more frequently in women with average age of 70 years.
Clinical picture: Episodic subacute obstruction in an elderly female. Abdominal pain and vomiting which subside as the gallstone becomes disimpacted, and only recurs again as the progressively larger stone lodges in the more distal bowel lumen. Intermittent symptoms may be present for some days prior to evaluation. Hematemesis could occur as an occasional complication that is due to hemorrhage at the site of the biliary enteric fistula.
Physical examination: The patient may be febrile and often appears dehydrated. Common abdominal signs include distension and increased bowel sounds. Jaundice is uncommon, occurring in less than 15% of cases. Many affected patients have serious concomitant medical illnesses, including coronary disease, diabetes mellitus or pulmonary disease.
Diagnosis: The most important diagnostic test is abdominal plain film. The diagnosis of gallstone ileus is made preoperatively in about one-half of cases. The radiographig findings of gallstone ileus, are:
- Signs of partial or complete intestinal obstruction
- Air in the biliary tree (pneumobilia)
- Direct visualization of the stone
- Change in position of a previously located stone
- Two adjacent small bowel air-fluid levels in the right upper quadrant
Treatment: First of all, as any kind of bowel obstruction, the objective is to relief intestinal obstruction after adequate fluid repletion. The options are enterolithotomy, cholecystectomy, and fistula division, with or without common bile duct exploration (one-stage procedure), with definitive repair performed at a second operation (two-stage procedure).
The treatment of choice is the enterolithotomy wich consits in localize and extract the gallstone. Often the cholecystectomy is contraindicated by comorbidities and the general state of the patient.
Case presentation: A 72 year old woman with heart faliure, hypertension and diabetes came to the office with a chief complaint of chills, abdominal pain, nausea and vomiting followed by inability to pass flatus 8 hours prior to consult.
On physical examination the patient was febrile and appeared dehydrated. Abdominal exam: distension and increased bowel sounds. No jaundice.
Labs: Hyperglicemia, mild renal failure, hypernatremia and leukocytosis.
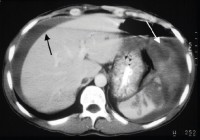
Radiographic tests: Abdominal plain film with signs of bowel obstruction and with not apparent cause, negative US. CT scan just with signs of intestinal obstruction, not pneumobilia, not obstructing gallstones.
The patient bacame hemodinamically unstable while performing the US and we decided to open her. On the OR we found the level of obstruction at terminal ileum and we felt a solid mass. We performed an enterolithotomy and the result was this:

Regards,
Dr. Jon Mikel Iñarritu