What is this?
Necrotizing Enterocolitis (NEC) is a syndrome wich consists in intestinal infarction.
What part of the intestine is affected?
Terminal ileum and colon, although the entire GI tract is affected in severe cases.
Why is NEC important?
Because NEC is the most common gastrointestinal emergency in the newborn infant and NEC accounts for substantial long-term morbidity in survivors of neonatal intensive care unit.
What are the risk factors of NEC?
Prematurity, milk feeding, circulatory instability, infection, and impaired mucosal defense. NEC incidence is greatest in newborn infants with birth weight less than 1.5 Kg, so prematurity is the most important risk factor.
How can be prevented?
It is well know that avoidance of hypertonic formulas, medications or contrast agents, prompt treatment of polycythemia, and placement of umbilical artery catheters with the tip below the level of the inferior mesenteric artery, prevent this condition.
What are the manifestations of NEC?
There are systemic and abdominal manifestations.
- Systemic signs are nonspecific and include apnea, respiratory failure, lethargy, poor feeding, temperature instability, or hypotension (in severe cases).
- Abdominal signs include distention, gastric retention (residual milk in the stomach before a feeding), tenderness, vomiting, diarrhea, and hematochezia (passage of bloody stools through the rectum).
How NEC is diagnosed?
The presence of abdominal distention, hematochezia, and pneumatosis intestinalis confirm the diagnosis of NEC.
We have to perform several studies, including blood analysis, stool analysis, sepsis evaluation, and radiographic studies.
The results of these studies often are nonspecific, although the radiograph may be diagnostic.
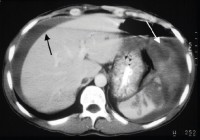
What are the findings at the radiograph?
Marked abdominal distention, dilated loops, pneumatosis intestinalis (bubbles of gas in bowel’s wall) and/or free intraabdominal air.
Could you show me a radiograph with this findings?
Yes, here you can see marked abdominal distention, dilated loops, pneumatosis intestinalis (bubbles of gas in bowel’s wall)

What is the treatment of this condition?
It depends on the stage of the disease. Medical managemente is appropiate in most cases, but in those patients with advanced NEC and bowel perforation we have to perform surgical intervention.
What are the complications?
The acute complications are infectious and hematologic. The late complications are intestinal narrowing or stricture formation and short bowel syndrome.
What is the prognosis?
Due to advances in neonatal intensive care, agressive treatment, potent antibiotics and earlier diagnosis, approximately 70% to 80% of infants who have NEC survive, and approximately 50% of these are normal. The mortality rate is higher in infants who require surgery for NEC.
Dr. Jon Mikel Iñarritu