Soriano’s Surgical Retractor in-action
2 Comments Published by Jon Mikel Iñarritu December 22nd, 2006 in Medical ImagesThis is the previously patented surgical retractor developed by Dr. Ángel Raúl Soriano Sánchez (Mexican Ob/Gyn from the National Institute for Social Security - IMSS) in action.
This amazing invention looks useful, isn’t it?
Hands transplantation
3 Comments Published by Jon Mikel Iñarritu December 14th, 2006 in Medical Images, NewsA 47 years old woman had both hands amputated 28 years ago. Now she is the first patient in Spain to receive a transplant of both forearms and hands.
This operation was done in La Fe Hospital in Valencia, Spain by the team of hand surgery of the Pedro Cavadas’ Foundation.
This is the 7th similar surgical procedure in the world and the first performed in a woman.
The patient will recover part of her sensibility in a period between five and six months.
State-Of-The-Art Surgery
3 Comments Published by Jon Mikel Iñarritu August 8th, 2006 in Medlinks, News, Daily Medical LifeFrom Medical News Today
Medical Center Accreditated by the American College of Surgeons:
The Beth Israel Deaconess Medical Center’s Carl J. Shapiro Simulation and Skills Center has been formally accredited as a Level 1 facility by the American College of Surgeons (ACS), the first in Boston and New England - and one of only six inaugural certified centers in the United States - to provide simulation-based skills training to health care students and professionals from all medical and surgical disciplines.
I would love to get that training.
Dr. Jon Mikel Iñarritu
Gallstone Ileus
11 Comments Published by Jon Mikel Iñarritu August 3rd, 2006 in Continuing Medical Education, Fast Facts, Medical ImagesGallstone Ileus is an infrequent cause of mechanical bowel obstruction. It is caused by an impaction of a gallstone in the terminal ileum by passing through a billiary-enteric fistula (often from duodenum). It occurs more frequently in women with average age of 70 years.
Clinical picture: Episodic subacute obstruction in an elderly female. Abdominal pain and vomiting which subside as the gallstone becomes disimpacted, and only recurs again as the progressively larger stone lodges in the more distal bowel lumen. Intermittent symptoms may be present for some days prior to evaluation. Hematemesis could occur as an occasional complication that is due to hemorrhage at the site of the biliary enteric fistula.
Physical examination: The patient may be febrile and often appears dehydrated. Common abdominal signs include distension and increased bowel sounds. Jaundice is uncommon, occurring in less than 15% of cases. Many affected patients have serious concomitant medical illnesses, including coronary disease, diabetes mellitus or pulmonary disease.
Diagnosis: The most important diagnostic test is abdominal plain film. The diagnosis of gallstone ileus is made preoperatively in about one-half of cases. The radiographig findings of gallstone ileus, are:
- Signs of partial or complete intestinal obstruction
- Air in the biliary tree (pneumobilia)
- Direct visualization of the stone
- Change in position of a previously located stone
- Two adjacent small bowel air-fluid levels in the right upper quadrant
Treatment: First of all, as any kind of bowel obstruction, the objective is to relief intestinal obstruction after adequate fluid repletion. The options are enterolithotomy, cholecystectomy, and fistula division, with or without common bile duct exploration (one-stage procedure), with definitive repair performed at a second operation (two-stage procedure).
The treatment of choice is the enterolithotomy wich consits in localize and extract the gallstone. Often the cholecystectomy is contraindicated by comorbidities and the general state of the patient.
Case presentation: A 72 year old woman with heart faliure, hypertension and diabetes came to the office with a chief complaint of chills, abdominal pain, nausea and vomiting followed by inability to pass flatus 8 hours prior to consult.
On physical examination the patient was febrile and appeared dehydrated. Abdominal exam: distension and increased bowel sounds. No jaundice.
Labs: Hyperglicemia, mild renal failure, hypernatremia and leukocytosis.
Radiographic tests: Abdominal plain film with signs of bowel obstruction and with not apparent cause, negative US. CT scan just with signs of intestinal obstruction, not pneumobilia, not obstructing gallstones.
The patient bacame hemodinamically unstable while performing the US and we decided to open her. On the OR we found the level of obstruction at terminal ileum and we felt a solid mass. We performed an enterolithotomy and the result was this:

Regards,
Dr. Jon Mikel Iñarritu
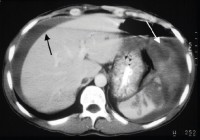
Splenic Injury and Hemoperitoneum in Blunt Trauma
5 Comments Published by Jon Mikel Iñarritu August 3rd, 2006 in Continuing Medical Education, Fast Facts, Medical ImagesThe following pictures are from different clinical cases.
In Blunt Trauma the spleen and the liver are injuried in 40 and 20 percent, respectively.
In the ER, you have three four options in the Work-Up of a patient with blunt abdominal trauma
- Peritoneal Lavage: Now just performed if you haven’t access to ultrasound (lack of money or lack of trained personnel). It’s indicated in specific cases, as in patients with cranial trauma, spinal trauma, for example.
Look the blood in the syringe and the tube. This is a positive peritoneal lavage due to blunt trauma.
- Ultrasound (a.k.a. FAST or Focused Abdominal Ultrasound for Trauma): This is one of the most used techniques, and should be performed for those patients hemodynamically unstables who can’t go to the coputed tomography room.
Look the irregular border. This is a positive FAST for hemoperitoneum due to blunt trauma.
- Computed Tomography: This technique has a magnific resolution for spleen, liver and vessels. Excellent evaluation for retroperitoneum. It has one inconvenience, hemodinamically unstable patients are not candidates for this analysis.
Black arrow = Hemoperitoneum.
White arrow = Injuried spleen
- Diagnostic Laparoscopy: Almost never recquired.
Look the blood in the abdominal cavity, this is a positive Laparoscopy for hemoperitoneum due to blunt trauma.
The controversy is when the hospital is not capable of performing the standarized protocol in blunt abdominal trauma (economic reasons), we doctors have to adequate to the circumstances and do our best effort.
For example, the first two photographs (peritoneal lavage) were taken at the Mexican Red Cross where money is the big problem. The rest, were taken at the ABC Medical Center, a nice private hospital. This are the contrasts of healthcare system and medicine practice in developing countries.
Regards,
Dr. Jon Mikel Iñarritu
Laparoscopic vs Conventional Nissen fundoplication
5 Comments Published by Jon Mikel Iñarritu July 19th, 2006 in Medical JournalFrom Annals of Surgery
A randomized trial that compares (subjectively and objectively) the laparoscopic versus conventional Nissen fundoplication in 5 years.
The comparision was made with 148 (79 laparoscopic vs 69 patients who were requested to fill in a questionnarie and to undergo esophageal manometry and 24 hours pH-metry.
Results: At 5 years follow-up, 20 patients had undergone reoperation: 12 after laparoscopy (15%) and 8 after conventional (12%). There was no difference in subjective outcome, with overall satisfaction rates of 88% (lap) and 90% (conv). Total esophageal acid exposure times (pH < 4) were 2.1% +/- 0.5% and 2.0% +/- 0.6%, respectively (P = 0.21). Antisecretory medication was taken daily in 14% and 16%, respectively (P = 0.29). There was no correlation between medication use and acid exposure and indices of symptom-reflux association. No significant differences between subjective and objective results at 3 to 6 months and results obtained at 5 years after surgery were found.
It concludes that the effects of laparoscopic and conventional are sustained up to 5 years and the long-term results are comparable. A substantial minority of patients in both groups had a second antireflux operation or took antisecretory drugs, although the use of those medications did not appear to be related to abnormal esophageal acid exposure.
I think laparoscopic approach is clearly superior due to the recuded hospital days and short convalescence period.
Regards,
Dr. Jon Mikel Iñarritu
Intussusception
0 Comments Published by Jon Mikel Iñarritu July 17th, 2006 in Fast Facts, Medical ImagesIntussusception is the invagination of a part of the intestine into itself, in other words is the prolapse of one part of the intestine into the lumen of an immediately adjoining part. It is the most common abdominal emergency in early childhood.
Epidemiology: Most episodes of intussusception occur in otherwise healthy and well-nourished children. Approximately 60% of children are younger than one year old, and 80 percent are younger than two. Is the most common cause of intestinal obstruction in children between 3 months and 6 years old. It appears to have a slight male predominance with a male:female ratio of approximately 3:2.
Etiology: The vast majority of cases is unknow. Another causes are Meckel’s diverticulum, polips, intestinal tumors, Henoch-Schönlein purpura, strange bodies, etc.
The most common form of this disease is the ileo-colic and ileo-ileo-colic invaginations. It could be associated with the rotavirus vaccine.
Clinical picture: Acute onset of intermittent, severe, crampy, progressive abdominal pain, accompanied by inconsolable crying and drawing up of the legs toward the abdomen. This painfull episodes occurs at 15 - 20 minute intervals and then become more frequent and severe. Vomiting may follow episodes of abdominal pain.
This episodes can be followed by vomiting and the passage of “currant jelly” stool (a mixture of blood and mucous). A sausage-shaped abdominal mass may be felt in the right side of abdomen. The prevalence of blood in the stool is as high as 70% if occult blood is included.
Diagnosis: It is based on index of suspicion, frequently the diagnosis is stablished with contrast studies (wich could be also therapeutic).
The abdominal plain film (see below) may be helpful because they may show frank intestinal obstruction or massively distended loops of bowel with absence of colonic gas.
The ultrasound can be useful also, with a sensitivity and specificity approach 100%. The classic finding is a “bull’s eye” or “coiled spring” lesion (see below) representing layers of the intestine within the intestine.
Treatment: Nonoperative reduction using barium or air contrast techniques is successful in approximately in 75 - 90% (in the first 24 hours) of patients with ileo-colic intussusception.
Surgery is indicated when nonoperative reduction is incomplete or when a persistent filling defect, indicating a mass lesion is noted. Broad-spectrum intravenous antibiotics should be given before surgery. Manual reduction at operation is attempted in most cases, but resection with primary anastomosis needs to be performed if manual reduction is not possible or if a lead point is seen.
Regards,
Jon Mikel Iñarritu, M.D.
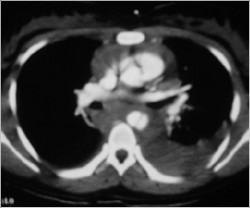
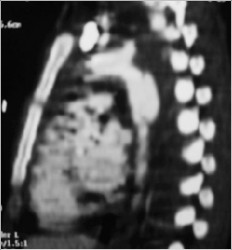
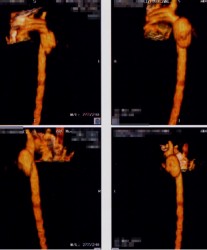
Traumatic thoracic aortic rupture
6 Comments Published by Jon Mikel Iñarritu January 23rd, 2006 in Medical ImagesA previously healthy 17 yo woman came in to the ER because she has suffer an automovilistic accident. On the initial evaluation she was with pulse ‘parvus et tardus’ with altered mental status. A chest x-ray was ordered and found an aortic rupture.

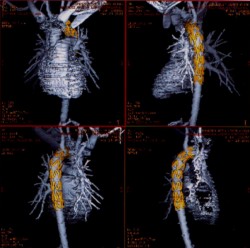
Because the bleeding was contained and she has just a little hemodynamic instability, the choice was endovascular treatment of traumatic thoracic aortic rupture.
A CT Scan was ordered preoperatory:
Endovascular Procedure
After Procedure
The outcome was excellent and the patient is in good shape rightnow with a normal lifestyle.
Regards,
Jon Mikel Iñarritu, M.D.










Recent Comments